Explaining STD- How Do You Get One?

Introduction
When I get that feeling I want sexual healing
Sorry Marvin. As the digital generation we’ve proudly done away with feelings, and have replaced them with STDs. You see, that common trope “catch feelings, not STDs”, is more applicable than ever now, because we’ve decided to catch trends, and jump on the dating app bandwagon.
You see, ever since we started sleeping around, wantonly, the floodgates of STDs have been opened up. It’s not so much sleeping around as it is sleeping around without protection or precaution.
When you contract an STD, there’s always that little shame that comes with things like “Ew, I can’t believe what I have” or “I wish I had known better". At the heart of every STD is denial - that you are not the target audience for an STD. That it should not have happened to you. Why, because “I am not that guy, bro”
“Raja ko rani se pyaar ho gaya” -But Rani only wants to be friends
Can you collectively hear the “hawwww” that reverberates through the room? We romanticise love. As a country, we are in love with the concept of love. Ask Shah Rukh Khan, bro.
He’s single-handedly made the nation swoon - and then feel all mushy about it. But sex? One second, what is this behaviour? We don’t go there! Haven’t you watched the classic Bollywood movies?
When a couple falls in love and wants to express it, the camera suddenly pans to flowers that come together. Milk boils over. There’s a quick shot of some buzzing honeybees. And then that’s it.
Unfortunately, from Bollywood to Instagram reels, love is painted in rose-tinted hues. There are violins in the background, some slow-mo twirls in mustard fields and the vague promise of eternal soulmates.
Cue Shah Rukh with one outstretched arm and a soft-focus lens. Also, add one fluttering curtain because it is better to flutter than stutter, right?
KKKKKIran wants to know your location.
Intimacy is not depicted in Indian cinema. It’s edited out. It’s as if the sex doesn’t even happen. Children come from e-commerce.
STD’s
STD, STIs, STFU - they’re all infections that come from one person to another via sexual contact. Whether it’s vaginal, oral or anal sex, you also get infected through skin-to-skin contact, shared needles, blood transfusion, etc depending on the infection. Common STDs are chlamydia, gonorrhea, syphilis, herpes, HIV and HPV.
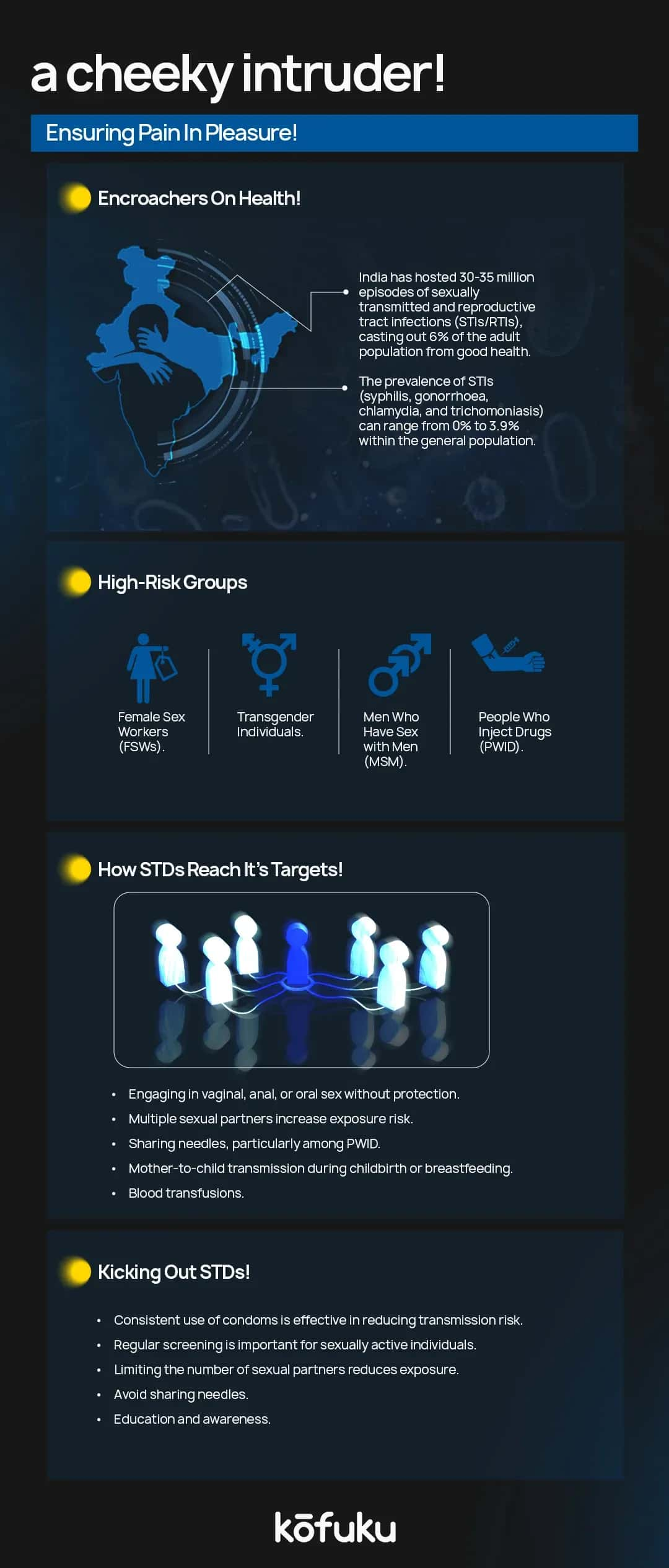
In India, the numbers speak for themselves. According to the National Aids Control Organisation (NACO), there are around 30-35 cases of STIs/RTIs annually. That’s nearly the population of a whole state, dealing with preventable and treatable infections.
And yet, people don’t talk about it. Sex is taboo. STDs are whispered about, laced with misinformation, shame, or good old-fashioned denial. Only the “promiscuous” people get STDs. The result? Infections slide undiagnosed, untreated, and continue to spread like neighbourhood gossip.
How Are STD Transmitted?
After how many dates does the protection come off? Asking for a friend.
Unprotected sex, whether oral, anal, or vaginal, is the most common way STIs spread. Each type of sexual activity comes with its own risk level, depending on the infection involved.
For instance, anal sex is risky in terms of HIV transmission because the rectum has a thin lining - that tears easier, permitting pathogens to enter.
Vaginal sex is the most common route of transmission for infections like gonorrhea, chlamydia and syphilis. Even oral sex isn’t risk-free (unless you use Colgate!). HPV, herpes, gonorrhea and syphilis - they all get transmitted this way.
The term “unprotected” usually means sex without a condom, or a dental dam, or feelings. Condoms bring down the risk, yes, but not fully. Infections like herpes and HPV can still spread through skin-to-skin contact, even if a condom is used. Durex, where are you?
The scary part is that people don’t show symptoms immediately or ever. You can pass on an STD to someone, and they wouldn’t even know, which is why routine testing and open conversations regarding sexual health are paramount.
If you are sexually active, protection, testing and honest dialogue should be a part of your health routine - unless you’re masturbating in a broom cupboard, in which case you can go back to doing what you were. Hello. Sex is natural. Protecting yourself should be natural, too.
Multiple Partners
Jaya, Sushma, Rekha aur Priya Sabki pasand chlamydia!
Infections spread, bro, like gossip. Ask us, city-slickers with multiple sexual partners. Guys and girls today are wearing their sexuality on their sleeves.
Having different sexual partners increases the risk of contracting and spreading STI. No one’s judging you; this is all about probability. The more partners you cycle, especially within short timeframes, the more likely you are to encounter someone carrying an infection. A lot of infections don’t have visible symptoms.
India is a curious country. Casual relationships and dating apps are common, but sexual health conversations and regular testing? That’s rare. One 2020 study, published in the Indian Journal of Community Medicine, showed how a lack of awareness and routine testing influences STD rates.
Use protection, bro and also get tested regularly - before starting a new sexual relationship. Honest, open communication matters. If you or your partner is polyamorous, be upfront. Be transparent, test regularly and use protection.
Sharing Needles
How many times have you chanced upon a heroin addict on the streets? Could be heroin could be any other drug, but trust me, the way that needle is sticking out of their arm, you can tell they haven’t been jabbing Rooh Afza.
From tattoos to body piercings, injecting drugs or more, is a high-risk route for transmitting sexually transmitted diseases. Such infections are bloodborne and passed from one person to another when dirty blood enters the bloodstream via reused or unsterile needles.
In India, this is a concern among people who inject drugs. The National AIDS control Organisation, NACO, tells us that nearly 6.3% of HIV cases in India are because of unsafe injecting practices. Drug use is not just the sole risk; unregulated tattoo parlours, informal piercing setups or rural clinics without proper sterilisation techniques.
Some people falsely believe that non-sexual means of transmission are not serious STI risks, but the lack of apparent symptoms in the primary stages of diseases like hepatitis C can result in long-term damage prior to diagnosis. Always visit certified professionals for inking, piercings or medical treatment.
Mother To Child Transmission
Newsflash. Sexually transmitted infections can also be passed on from a mother to her child, either during pregnancy, childbirth or breastfeeding - this is called vertical transmission.
Meanwhile, all Raja Betas in the house go like “Aye, my mother only gave me issues, not infections”.
Believe me, though, this mode of transmission is often overlooked in public discussions, but they remain a concern, especially in countries like ours, where maternal healthcare access is - nonexistent.
Still, UNICEF tells us that more than 22,000 children were newly infected with HIV in India as of 2021, a lot of them through mother-to-child transmission.
Without timely screening and treatment, STIs in pregnant women can result in miscarriage, premature birth or even stillbirth, or worse, health complications in newborns.
The good news? With early intervention, this is preventable. It’s called routine antenatal screening for STI. In case of HIV, consuming antiretroviral drugs while you are pregnant can bring down transmission rates.
Awareness - cause God knows we lack some!
Blood Transfusions
Earlier, STIs would spread through blood transfusions, but since we banned poor people from hospitals, that bit has been solved. Oh wait.
Even today, transfusion is a potential route for transmitting certain infections like HIV, hepatitis B, C and syphilis. Before we denied poor people healthcare, they were spreading AIDS like gossip, bro.
Just for perspective, 12 million blood units are collected annually. There’s even a National Blood Policy, which mandates mandatory screening of donated blood for most infections. The WHO has said that some centres are ill-equipped to carry out tests.
Things get worse when people turn to unregulated or illegal blood banks, thanks to desperation or lack of access. Unsafe transfusion can happen anywhere, so keep your eyes open.
To stay safe, stay away from Government hospitals no? No? Seek medical care from licensed, well-equipped hospitals, where the sourced blood is screened.
Skin-to-skin contact
“No penetration, only potential viral transmission”
A lot of people are misinformed and claim that sexually transmitted diseases only spread through penetrative sex. Well, until you reach 3rd base. Skin-to-skin contact can spread infections.
Notably, infections like Human Papillomavirus (HPV), herpes simplex virus (HSV), molluscum contagiosum, and syphilis can spread simply through intimate contact with infected skin or mucous membranes.
In India, awareness of such routes is low. Studies claim that less than 20% of sexually active young adults even know how an STI spreads. They “fool around” because it’s risk-free. Not true.
Physical intimacy - no matter how mild - is full of risks - don’t you know that?

Who Is At Risk?
Okay, let’s get one thing straight. If you are sexually active, you are at some level of risk for sexually transmitted diseases.
It doesn’t matter whether you have had one partner or many. STI will not discriminate - they don’t care about your relationship status, gender, or how many followers you have on Instagram.
So, who is vulnerable? Adolescents and young adults. Because of lack of sex education (We’re Indians. Our sex education came from porn sites), impulsive decision-making and the whole “it cannot happen to me”.
Sex workers are particularly vulnerable. They have limited access to regular health check-ups. They face higher exposure because of the frequency and diversity of partners. Also, men who have sex with men (MSM) are at an increased risk for particular infections, especially where you’d rather die of AIDS than seek help.
Then come polydrug users. Sharing needles is dangerous - it’s like you’re inviting STDs.
But here’s the catch - such risks are well-managed or even eliminated. The aim is to stay informed, shatter the stigma and protect yourself and your partners.
Common Myths About STDs
When it comes to STDs, myths are more contagious than the infections. One myth is that you can only get an STD if you are promiscuous. That’s right.
Introverts, without Intercourse, so no issues there.
Hey! That’s not true.
You can get an STD by reading Women’s Era.
People with one sexual partner - if you aren’t using protection, be aware. Safe sex is not a myth. Do it. Also, oral sex is not completely safe.
Toothpaste will kill the bacteria in your mouth, not on someone else’s peepee.
Just because there’s no penetration doesn’t mean it’s risk-free. Condoms and dental dams can go a long way in bringing down the risk.
Also, if you think you can get away and not get an STD, just because you have no symptoms, think again. HPV and chlamydia don’t show symptoms, but that doesn’t mean you are STD-free.
Another myth is that STDs always show symptoms - in truth, most infections lie dormant and show no signs till complications show up. Don’t wait for symptoms - it’s not like your electricity bill.
We have to bust such myths because they prevent people from getting the care they need. They also add unwanted shame to a subject that has already been stigmatised. Let’s replace judgment with awareness - to create a culture where sexual health is treated as a normal, important part of well-being.
Protecting Yourself
Q-What’s the height of safe sex?
A-Masturbating with a condom on.
Want to protect yourself from an STD?
Don’t have sex. Simple
Still here? Read on.
Always use protection - condoms, dental dams and the works. Vaginal, oral or anal sex - barriers can bring down your transmission chances.
If you are sexually active, especially with new or multiple partners, you should undergo routine STD testing. Lots of infections have no symptoms, so testing is the only way you’ll know.
Open communication is also important.
Ladies, if you’re asking him how much money he makes, also ask him about chlamydia.
Conversations about sexual health build trust and keep everyone safer.
Also, stay away from alcohol.
You get risky after drinking whisky.
Your sexual health is part of your overall well-being—protect it, normalise it, and own it.
What Do You Do If You Think You Have *insert STD here*
If you think you have an STD, go to a doctor. Like right now. Don’t panic and Google. Or pray. Maybe not. God doesn’t want to have anything to do with your privates, bro.
A qualified healthcare professional, who can guide you with the right tests and treatment, is the best way to go. Most STDs are completely treatable. When they aren’t curable, like HIV or herpes, they can be managed effectively using medication and regular monitoring.
Your privacy is protected. Healthcare providers are bound by confidentiality, so speak, and thou shalt not be judged. Don’t self-diagnose or self-medicate- this can make things worse and delay treatment.
Also, stop having sex until you’ve seen a doctor and are clear about your status. That’s the least you can do for you and your partner. Getting tested isn’t bad; it makes you aware.
Awareness is power. It’s just routine self-care. Just like you won’t ignore a persistent cough or rash, don’t ignore your sexual health. Prioritise it, own it and respect it.
STDs in India: The Real Picture
When I was growing up, STD meant outstation phone calls.
STDs remain a major health concern in India, affecting millions annually. Recent data tells us that around 30 million people contract STDs every year, which means that these infections are widespread, bro.
The Indian government has the National AIDS Control Organisation (NACO) has more than 1160 designated STI/RTI clinics, called Suraksha Clinics, across India. You get free, standardised services, including counselling and treatment for STDs. No judgement.
Challenges persist, though. One barrier is the stigma that comes with STDs, which discourages individuals from seeking timely medical attention. Also, misinformation about transmission and prevention contributes to the spread of such infections.
What makes this worse? Disparities in healthcare access across urban and rural areas. In rural areas, individuals have to travel far to reach healthcare facilities, with most medical costs paid out-of-pocket. This limited access, together with lower education and awareness levels, results in more STDs in rural populations.
Addressing the STD epidemic in India will take a multifaceted approach - we have to boost public awareness, kill stigma, improve accessibility to healthcare services, and make sure education is consistent, everywhere. Education is important- just ask Haryana.

Conclusion
Sexually transmitted diseases are more common than most people think - and far less talked about. Nowhere else has silence ensured such lasting damage. The only way we can bring down the spread is by normalising conversations around them.
Contracting an STD doesn’t make you dirty or immoral. It just means that you were human, and you had sex. The infection is not the danger - the lack of awareness, stigma and inaction are.
Most STDs are treatable, some curable, and all are manageable - if you diagnose them early. Just take ownership of your sexual health. Use protection. Get tested. Talk openly. Because you know what spreads faster than infection? Awareness.
FAQs
Q. What are the most common STDs in India?
A. Some of the most common STDs in India include HIV/AIDS, gonorrhea, syphilis, chlamydia, and herpes.
Q. Can I get an STD even if I’m not promiscuous?
A. Yes, STDs can be contracted by anyone who is sexually active, even with one partner. It's important to remember that the presence of an STD is not a reflection of your character or promiscuity.
Q. Are STDs always visible or symptomatic?
A. No, many STDs don’t show visible symptoms, especially in their early stages. That’s why regular testing is crucial.
Q. How can I prevent STDs?
A. Using condoms consistently and correctly during all types of sexual activity (vaginal, anal, and oral), getting vaccinated for HPV and Hepatitis B, and regular screening are key methods of preventing STDs.
Q. What should I do if I think I have an STD?
A. If you suspect you have an STD, please add ISD and PCO.

69 Fun Facts about Sex that you did not know

Breaking the Taboo Around Sexual Health – Let’s Discuss

Let’s Talk Sex Toys: Do You Need Them?

Understanding Hypersexuality: When It’s Too Much

How to Practise Safer Sex? Know Before You Face Consequences


