H5N1 Virus: Global Virus Network Warns of Potential Pandemic

Introduction
Time for all of us to go back to hoarding toilet paper again, it seems!
The United States is experiencing an unprecedented H5N1 virus outbreak that has so far impacted nearly 1,000 dairy cow herds and led to over 70 human infections, including the first confirmed death in the U.S.
The scary part is that the virus has transmuted to infect mammals with the possibility of human-to-human transmission.
The Global Virus Network, an international coalition of leading medical virologists from over 40 countries, has published an urgent call to action. The message is clear - we need strong disease surveillance, strict biosecurity measures, and serious preparation in case the virus makes that next leap of human-to-human transmission.
What is H5N1 — and Why Are Experts Worried?
Let’s break it down.
Flu viruses come in three basic types: A, B, and C. Type C causes the mildest illness. Type B can make you feel just as awful as Type A, but it’s never been responsible for a global pandemic. That job, unfortunately, belongs to influenza A - the only one of the three that’s managed to wreak havoc worldwide.
Now, within influenza A, there are a whopping 144 different subtypes - from H1N1 to H9N16. All of them circulate naturally in wild birds, which means technically, they’re all bird flu. Most of the time, they stay in birds.
But every now and then, one of these viruses mutates just enough to start infecting other animals, and that’s when things get risky. H5N1, specifically the variant known as 2.3.4.4b, has virologists and public health officials on high alert and here’s why.
First, H5N1 2.3.4.4b is what scientists call “highly pathogenic.” That means it doesn’t just infect animals - it makes them very sick, and in many cases, it’s fatal. Wild birds, poultry farms, and even mammals are being hit hard.
But here’s the bigger concern: this virus is evolving. And fast. It’s no longer just a bird flu. It’s showing an alarming ability to jump species - including to mammals, which suggests it’s getting closer to being able to infect humans more efficiently.
The United Nations’ Food and Agriculture Organisation has described the spread of H5N1 as “unprecedented,” warning that its reach is now threatening not just animal health, but global food security and economic stability too.
Some experts are even warning that if H5N1 continues on this path, it could spark a pandemic worse than COVID-19.

How Does It Spread?
H5N1 is what scientists call a highly pathogenic avian influenza (HPAI) virus. That means it spreads quickly and causes serious illness, especially in birds. This isn’t just a problem for wildlife but a major challenge for food security and has been devastating for the poultry industry in many parts of the world.
In birds, the virus is mainly spread through saliva, nasal secretions, and droppings. Domestic poultry like chickens are especially vulnerable. Migratory wild birds can carry the virus across continents, making it hard to contain.
But the virus hasn’t stopped with birds.
When sea mammals like seals and sea lions ate sick or dead birds, they too became infected. On land, foxes and raccoon dogs have caught the virus as well. By the end of 2022, H5N1 had jumped to farmed mink, possibly through exposure to infected waterfowl, and soon after, cases began to appear across the United States.
Then, in March last year, the virus made another leap into dairy cattle. The initial transmission likely came from infected bird droppings or mucus, but once in the herd, it began spreading between cows, probably through shared milking equipment.
Fast-forward to 2025, and H5N1 is now widespread across Europe, Asia, South America, and the US. It’s tearing through the poultry and dairy industries, causing both economic and animal welfare crises.
Even more concerning? It’s showing up in unexpected places.
In the UK, the virus was found in a sheep on a Yorkshire farm, and it even made its way into the sheep’s milk. In the US, unpasteurised milk has been found to contain high levels of the virus. Cats that roam near dairy herds have become infected after sneaking a few drops, and raw pet food has also been linked to cases.
And yes, humans are getting infected, too.
In January, a man in the US died after catching H5N1 from his backyard chickens. When scientists analysed his blood, they discovered something deeply concerning - the virus had already begun to mutate in ways that could help it better infect humans. Just a month later, three US veterinarians working with dairy cattle also tested positive.
The silver lining? For now, H5N1 still doesn’t spread easily between humans.
Unlike COVID-19, which spreads through the air, H5N1 2.3.4.4b is primarily transmitted through direct contact with infected secretions or by ingesting things like raw milk or contaminated meat.
So far, of the 70 recent confirmed human cases in the US, only one has resulted in death.
Symptoms of H5N1 in humans
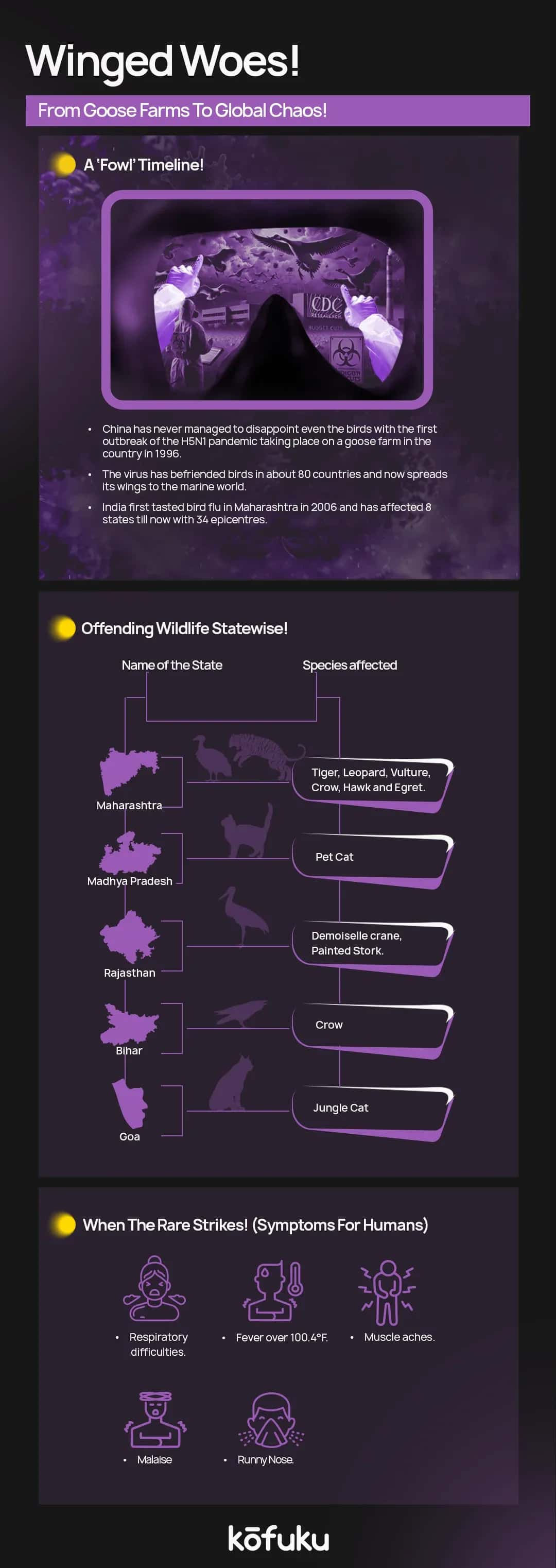
H5N1 infection can start like regular flu - think high fever (over 38°C), cough, sore throat, muscle aches, and fatigue. Some people also get conjunctivitis or other early non-respiratory symptoms.
But unlike typical flu, it can turn serious fast. In severe cases, it leads to pneumonia, acute respiratory distress syndrome (ARDS), neurological symptoms (like confusion or seizures), and even multi-organ failure.
Some patients have reported diarrhoea and encephalitis, too.
One of the biggest concerns with H5N1 isn’t just the illness itself - it’s the potential for the virus to change. In the winter months, especially in the northern hemisphere, human flu viruses and H5N1 can circulate at the same time.
If someone were to get infected with both at once (for example, a human flu virus and H5N1), the viruses could mix. This is called reassortment, and it could create a new strain that spreads more easily between people, which is exactly what experts fear could trigger a future pandemic.
So far, that hasn’t happened - but it’s one reason health officials are watching it closely.

Conclusion
There’s a lot of cause for concern. There needs to be effective protocols, stricter regulations, and more food security. But what can we do in the meantime?
Stay informed. Don’t eat raw or undercooked meat, eggs, or unpasteurised milk, especially from areas with bird flu outbreaks. Boil milk if it's not pasteurised. Avoid contact with sick birds, bird droppings, or dead animals.
Make smart, safe food choices.
H5N1 is serious, and the risks are growing. But it’s about being aware, not alarmed, and doing what we can to reduce risk.
FAQs
Q. When was the first H5N1 outbreak?
A. The first H5N1 outbreak was reported in poultry in Scotland.
Q. How does H5N1 spread to humans?
A. Humans typically get infected through direct contact with infected birds, their droppings, or contaminated environments, not through cooked poultry.
Q. What are the symptoms of H5N1 in humans?
A. Common symptoms include high fever, cough, sore throat, and difficulty breathing. It can lead to severe respiratory illness and even death.
Q. Is there a vaccine or treatment for H5N1?
A. There is no widely available vaccine for the public, but antiviral medications like oseltamivir (Tamiflu) may help if taken early.
Q. How can I protect myself from H5N1?
A. Avoid contact with sick or dead birds, practice good hygiene, cook poultry thoroughly, and follow public health guidelines.

What Is Human Metapneumovirus? Learn More

Wetlands Virus: Is It the Next Big Thing After COVID-19?

Impact of Contagion on Healthcare Systems and Policies

All You Need to Know About How Contagion Shapes the World

The History, Impact, and Importance of Vaccines Worldwide


