Can Managing Emotions Help Us Control Chronic Pain? A Deeper Dive

Introduction
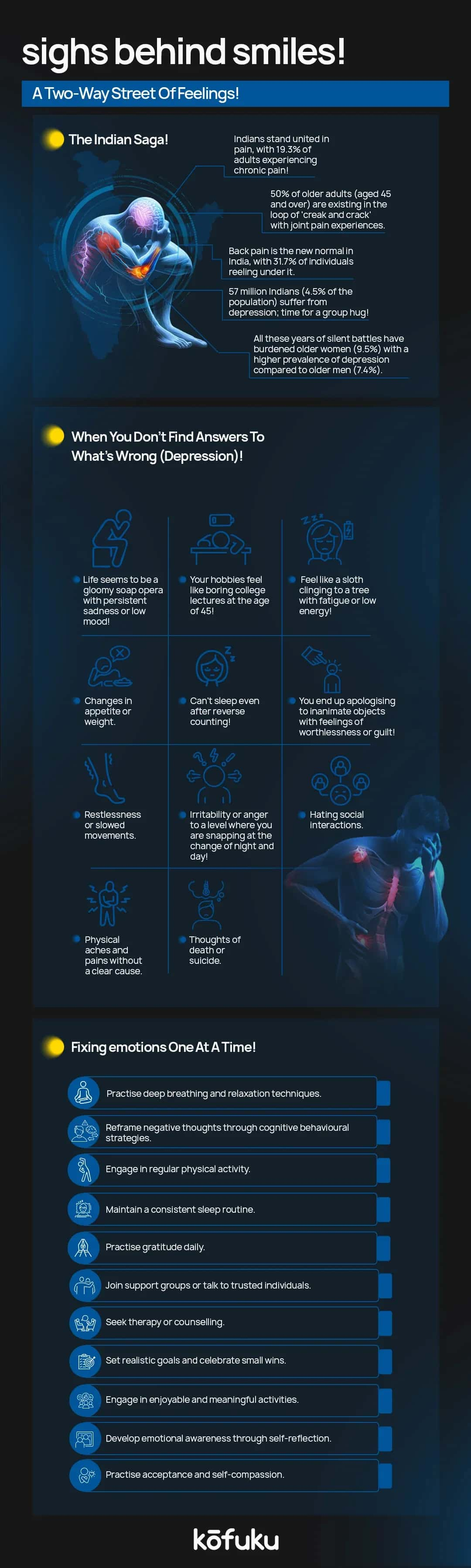
No matter what we say, our world's mental and physical aspects are closely related. It should be no wonder that emotional states affect physical pain. Chronic pain doesn’t just impact the body - it takes a huge toll on the mind.
When pain stays beyond the regular stipulated healing time, it can result in emotional distress, with depression arising as one of the most common comorbidities.
According to research, there are overlaps in the biological mechanisms behind both depression and chronic pain, such as neurotransmitter imbalance, inflammatory responses and brain chemicals such as Brain-Derived Neurotrophic Factor and glutamate.
In this article, we will explore how shared molecular pathways can lead to more targeted treatments. It will also touch upon how emotional regulation and mental health awareness play vital roles in managing chronic pain better.
Science is constantly uncovering further links between mind and body. Emotional well-being is quickly emerging as a vital tool in the battle against long-term pain. In this article, we will explore science, psychology, techniques, and real-world applications.
Understanding Chronic Pain
Chronic pain is not simple. It’s a web of facts, lies, and more- a complex condition that carries on for weeks, or even years, long after the original injury has healed. Don’t confuse this with acute pain - that is something you can get rid of with a spray of Moov or Iodex.
Chronic pain is when you’ve run through your fifth can of Iodex spray while your hip still feels like a horse danced on it. Time to write a strongly worded email to the CEO of Iodex.
“Brooo, this is not working bro!”
And oh. CC God.
Coming back to chronic pain, it lasts for three months or longer, sometimes without a clear issue. Because of this lingering nature, diagnosing and treating this sort of pain is difficult, spurring ongoing research into its myriad underlying mechanisms.
Let us first consider the biological level. Pain begins when nociceptors - specialised sensory nerve fibres in the skin- pick up harmful stimuli and send signals to the brain and the spinal cord. Such signals might carry on in chronic pain even without ongoing tissue damage.
Aspects like neuropathic (nerve-related), nociceptive (injury-related), and neuroplastic (brain-related) changes result in this prolonged pain experience.
The body has a pain regulation system involving descending inhibitory pathways that block pain signals in the spinal cord.
When these pathways malfunction, the perception of pain increases manifold. Inflammation also plays a vital role in chronic conditions like migraines, arthritis, and back pain, where immune cells boost nerve sensitivity and prolong pain responses.
Beyond affecting just the body, chronic pain impacts daily life. People struggle with sleep disturbances, strained relationships and reduced mobility.
They can’t hold down a steady job. And let’s not even get started on the emotional burden, as ongoing pain is closely related to depression, anxiety, irritability, and feelings of hopelessness.
So, what are the common types of chronic pain? Lower back pain, migraines, fibromyalgia and arthritis. We have to break down the biology behind pain.
All we need to help people regain control over their lives is growing awareness and research, more integrated treatment options, and a lot of luck.
The Mind-Body Connection
Chronic pain and depression are closely linked, via overlapping molecular and neurological mechanisms that come together to create a powerful mind-body connection.
The brain decodes pain signals via a network of pathways, including the thalamus, spinal cord, and third-order neurons. However, the limbic system, which is the brain’s emotional centre, plays an indispensable role in modulating how such signals are experienced.
When emotions like anxiety, fear or hopelessness are activated, they can boost pain perception by changing limbic processing.
Such interactions are further heightened by central sensitisation, a state in which you have a hyper-reactive nervous system, misfiring pain signals even when real tissue damage remains absent.
Molecular factors, like monoamine neurotransmitter depletion, BDNF dysregulation, inflammatory cytokines and glutamate receptor activity, give rise to this hypersensitive state.
Scientific studies have time and again shown that constant pain can bring down dopamine activity in the midbrain and bring down D2R receptor expression, a characteristic of both depressive disorders and chronic pain.
Also, inflammation-encouraged changes in neurotransmitter metabolism, epigenetic changes like histone acetylation and DNA methylation, and reduced adult hippocampal neurogenesis, further emphasise this shared pathology.
Emotional distress and chronic pain just don’t coexist; in fact, one biologically intensifies the other, giving rise to a feedback loop that can make both conditions harder to treat. What do we need?
Integrative approaches that look at both emotional and physical aspects of chronic pain.

How Emotions Influence Pain
We have to wrap our heads around the epidemiology of chronic pain - how else would we tackle its widespread impact?
The International Epidemiological Association defines epidemiology as the study of health-related events and their determinants in populations.
Chronic pain, once sidelined as a symptom or comorbidity of other illnesses such as depression, heart disease and stroke, is now factored as a condition in its own right, with a whole lot of risk factors.
There was a large-scale telephone survey conducted across eight major Indian cities, that showed us that 13% of respondents are suffering from chronic pain with the knees, joints and legs being the most commonly impacted areas.
Also, those living with chronic pain have deteriorating social relationships and diminishing independence, which shows how severely this condition can impact every aspect of daily life.
But yeah, it’s not as if physical discomfort is the be-all and end-all of this. Emotional well-being is closely tied to the pain experience.
-
Stress and pain - When the body is stressed, it releases adrenaline and cortisol, hormones that can boost pain perception by sensitising the nervous system.
-
Depression and chronic pain - This is a bi-directional relationship - chronic pain can result in depression, and depression can worsen the intensity and duration of pain.
-
Anger, fear and frustration - When these come about, physiological responses that tighten muscles, bring down pain tolerance and boost inflammation - fueling the pain cycle.
-
Neuroplasticity - Emotional states just don’t influence momentary pain - they can rewire the neural pathways over time, resulting in long-term changes in how pain is processed and regarded.
This burgeoning body of research only goes to show that pain isn’t just physical - it’s emotional and neurological as well. Addressing emotional health is hence just as important as medical treatment in tackling chronic pain.
Is Emotional Regulation The Way Forward?
What is emotional regulation - it’s basically managing and responding to emotional experiences albeit in a healthy and constructive manner.
You have to be cognizant of emotionalism, comprehend them and employ strategies to influence just how and when emotions get expressed.
For folks living with chronic pain, emotional regulation goes beyond coping skills - it is an indispensable aspect of pain management.
How does emotional regulation work? It does so by bringing down the fight-or-flight response. Chronic pain often activates the stress systems of the body, boosting cortisol and adrenaline levels. What does this spur?
It leads to increased pain sensitivity, muscle tension and a compromised immune function. Emotional regulation techniques, like slow breathing, cognitive reframing or mindfulness - can help restore some calm, bring down sympathetic overactivation and goad the body into a more balanced state.
Such a physiological shift can bring down pain intensity and boost overall resilience.
But don’t believe us just because we said so. Research supports such effects as well. Clinical studies have exhibited that people who dabble in emotional regulation techniques have a marked reduction in pain perception and distress.
A 2010 study published in The Journal of Pain, tells us that participants practising mindfulness-based stress reduction show remarkably lower pain intensity and better overall emotional well-being as opposed to say a control group.
Other studies have shown us that therapies like cognitive behavioural therapy (CBT) can bring down the emotional reactivity linked to chronic pain, making it more manageable and less intrusive to daily life.
There have been real-world examples that vouch for the power of emotional regulation. One patient with fibromyalgia started “daily journaling” to track emotional triggers and responses.
Over time, she found that tackling suppressed emotions and reframing her thoughts brought down flare-ups. Another person, suffering from chronic back pain, fused mindfulness meditation and guided breathing exercises into his routine.
The result? Decreased pain episodes and improved mobility after just a few weeks. Therapy, especially CBT and acceptance and commitment therapy (ACT), has also assisted patients in developing better self-awareness, bringing down pain-related anxiety, and regaining a sense of control.
Techniques that Actually Work
But what works? For emotional regulation, that is? How on earth are you going to diminish chronic pain, what with all those random emotions flying around? Okay, let’s decode this once and for all.
You see, chronic pain isn’t just physical but also deeply tied to thoughts, behaviours and emotions.
Different mind-body techniques have exhibited promise in assisting individuals in managing pain by targeting the emotional and psychological responses that mostly exacerbate it.
Given below are some evidence-backed approaches that support emotional regulation and can result in meaningful reductions in pain intensity and emotional distress.
Cognitive Behavioural Therapy
Okay, let’s get the most obvious one out of the way first. The reason CBT is so famous is that it's effective. Period. It can help you identify and reframe bad or catastrophic thoughts related to your pain.
For instance, a person who constantly ruminates “This pain will never subside” might experience more hopelessness and distress, which worsens the perception of pain.
CBT tackles such automatic thoughts, replacing them with a balanced perspective instead. So you say, “This pain is hard, but I have the tools to manage it”. As time goes by, this cognitive shift reduces pain-related fear and boosts functioning.
Mindfulness and Meditation
Move over, medication. It’s time for meditation, which brings gentle, non-judgmental awareness to the present moment. Don’t resist or fear the pain. Notice physical sensations, yes, but don’t attach negative meaning or emotion to them.
Studies have shown that proper mindfulness meditation can bring down pain perception, reduce emotional reactivity and bring down levels of stress hormones. Body scans, guided meditation and mindful breathing are great tools for fostering acceptance and calm.
Acceptance and Commitment Therapy (ACT)
Move over CBT, it’s time for ACT - that stresses accepting pain instead of struggling against it. The goal? To shift from a life dominated by pain avoidance to one guided by meaningful action and personal values.
For instance, someone who avoids walking due to discomfort might go through ACT and start short daily walks because being active is good for health and independence. This reorientation helps diminish the emotional suffering surrounding pain while fostering psychological flexibility.
Breathe - It Costs Nothing
Chronic pain often triggers a stress response in us, activating the sympathetic nervous system, our “fight or flight”.
Techniques such as deep diaphragmatic breathing, guided imagery and muscle relaxation can stimulate the parasympathetic nervous system, which calms the body and boosts healing.
Slowing the breath can bring down muscle tension, anxiety and heart rate - all of which result in a lower perception of pain.
Expressive Writing-Emotional Awareness
Unprocessed emotions like trauma, anger or grief can give rise to chronic pain. Expressive writing gives us a safe space to explore and articulate such emotions.
Journaling puts forward unconscious stressors, making it really easy to get rid of them. Write about your feelings and thoughts - it can improve your mood and physical symptoms.
It also fosters emotional awareness, so individuals can recognise triggers and patterns linked to their experience of pain.

Emotional Management and Pain Treatment - The Integration
Move over medication -it’s time to treat the physical sources of pain, especially when it's chronic.
According to research, emotions like anxiety, fear, stress and depression can exacerbate the perception of pain and even mess with healing.
Why do you think more and more healthcare providers are moving towards a more integrated care model that includes emotional regulation as an important part of pain management?
Psychologists and pain specialists come together in multidisciplinary pain clinics, giving patients a rather robust treatment experience.
Shrinks guide patients in thought exploration, emotional and behavioural interactions with their physical symptoms. Pain specialists, meanwhile, bring their best foot forward with interventional treatments and medical management.
The result? A coordinate plan that treats the person as a whole, not a bunch of symptoms.
Ignore the emotional dimensions of pain and you’re in for trouble - prolonged suffering, emotional burnout and even unfavourable physical outcomes pose real consequences.
For instance, anyone who is dealing with unsolved grief or trauma will tense their body, further encouraging muscle pain or headaches. Sans emotional insight, treatment is half-baked and usually useless.
Then there are multidisciplinary clinics that offer the advantage of clubbing medical expertise with physical therapists, and other specialists, all under one roof. Team based, this approach results in superior clinical outcomes but also helps patients.
Time to do away with the isolation cycle that most people with chronic pain go through - instead, now let’s tackle this pain with tools for self-care.
Whichever way you look at it, effective pain management is a shared responsibility. While healthcare systems might give you access to integrated services, patients also do well because they actively engage their emotional well-being, either through therapy, support group and mindfulness.
Our goal? Reduce pain yes, but also exercising a modicum of control to improve the quality of everyday life. Holistic pain removal is also one-step for caring for the mind just as much as the body.
Challenges and Misconceptions
Let’s face it. There’s awareness about the mind-body connection. However, tons of misconceptions still stop people from completely embracing emotional management as a part of pain treatment.
One of the most damaging is the messed-up belief that chronic pain is “all in your head”. This stigma invalidates the real, physical experience of pain but also stops people from seeking emotional support.
The brain plays a vital role in our perception and processing of pain and emotions can majorly influence that perception.
Cue cultural norms and values - that can also act as barriers. In many communities, emotional expression is a sign of weakness.
People are taught to “tough it out” or “remain strong”, making them suppress their emotional struggles.
This intransigence to emotional openness can worsen psychological distress and exacerbate physical symptoms as time goes by, perpetuating a vicious cycle that is difficult to break - unless you have support.
Another myth - mind-matter techniques are sufficient to conquer chronic pain. Okay, there are emotional tools like meditation, therapy and journaling. However, they’re not magic bullets.
Don’t replace physical treatments like physiotherapy, medications or surgical interventions with them. Emotional management is a crucial addition - an extra layer of support that bolsters the efficacy of physical treatments.
Pain is not imaginary or psychological. Emotional well-being plays a vital role in recovery. By addressing and acknowledging such challenges and misconceptions, we can change the narrative around chronic pain and turn it into a more compassionate, informed and integrated approach.
Patients deserve a treatment plan that validates their physical, emotional and every other experience.
Conclusion
To sum up, chronic pain goes beyond being physically hurtful - it is a complex interplay between mind and body. The emotional landscape of a person in constant pain profoundly shapes how that pain is experienced, endured and managed.
The age-old belief that “it’s all in your head” invalidates the legitimate, physiological role that emotions play in increasing or alleviating pain. It ain’t mind over matter - it’s mind with matter.
Clinical research supports this. Pharmacological treatments, like opioids, benzodiazepines, and antidepressants, remain essential tools, especially for neuropathic and cancer-related pain, but they come with risks like dependency, cognitive dysfunction, and reduced emotional resilience.
The careful use of antidepressants like SNRIS and tricyclics shows potential, yet none proffer up a holistic solution. Also, psychotherapy has emerged as a powerful ally.
Both CBT and CFT reframe how patients perceive and respond to pain, giving rise to more adaptive behaviours and mitigating the psychological burden that more often than not accompanies chronic discomfort.
FAQs
Q. Can emotions really make chronic pain worse—or is that just in our head?
A. Not at all, “just in your head.” Emotions like stress, anxiety, fear, and sadness have real biological effects. They can change how pain is processed by the nervous system, making it feel more intense. Think of it like turning up the volume on a radio—your body interprets pain signals louder when emotional distress is in the mix.
Q. How does emotional regulation reduce physical pain?
A. Emotional regulation helps by calming the body’s stress response. When you breathe deeply, reframe your thoughts, or practice mindfulness, you’re activating the parasympathetic nervous system (the "rest and digest" mode), which reduces cortisol and adrenaline. This shift lowers inflammation, relaxes muscles, and decreases your overall pain sensitivity.
Q. Is therapy really effective for managing chronic pain?
A. Yes - especially therapies like CBT (Cognitive Behavioural Therapy) and ACT (Acceptance and Commitment Therapy). These aren’t about “curing” the pain, but about changing your relationship with it. They help you develop coping strategies, reduce catastrophic thinking, and improve your emotional resilience, which in turn can significantly ease pain intensity and its impact on your life.
Q. What’s more helpful—medication or meditation?
A. Both have their place, but meditation offers something unique—Baba Ramdev will personally come and oversee your practice session. Jokes apart. Practices like mindfulness help you notice pain without emotionally reacting to it. Over time, this changes neural pathways and reduces chronic pain perception. Plus, no side effects. You can even start with just 5 minutes a day.
Q. I’ve tried everything. What makes emotional regulation worth a shot?
A. Unlike quick fixes, emotional regulation builds long-term resilience. It doesn’t just address pain, but the way you experience and respond to it. Techniques like journaling, breathwork, and guided imagery can empower you, giving you back a sense of control. And when chronic pain feels less like a bully and more like a background hum, you’ve already won half the battle.