Irritable Bowel Syndrome vs Inflammatory Bowel Disease


Introduction
There she was, hanging out with her friends after a long break, finally at the cute little bar they’d been planning to visit for weeks. The spicy ramen was the main attraction, the very main reason customers kept coming back.
The girls figured, why not give it a try? But just as she took a bite, our protagonist heard the ominous sounds coming from her stomach. Gurgles, twists, and a clear threat of betrayal on a girls' night out? (Oh, hell no!)
Without warning, she made a dash to the nearest bathroom, like a scene straight out of Mission: Impossible (1996).
Now, the thing is, does this sound familiar to you? If so, then welcome to the club nobody wants to join. Way too many people are in this group, “the Poopie Issue Group.” Not all tummy tantrums are created equal.
Come along as we discuss Irritable Bowel Syndrome and Irritable Bowel Disease. They may sound like evil twins, but you’d be surprised to know they attack differently.
What Are Irritable Bowel Syndrome and Irritable Bowel Disease?
Let’s begin with what Irritable Bowel Syndrome is.
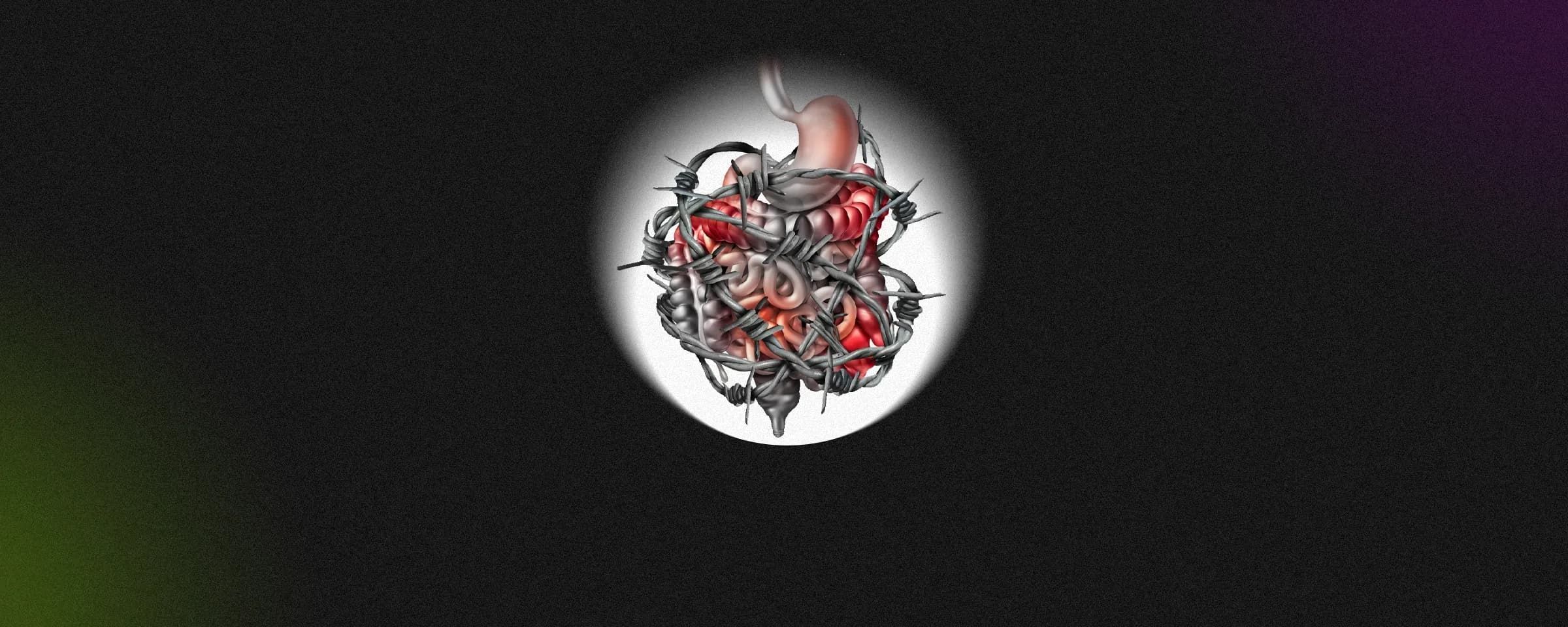
IBS (Irritable Bowel Syndrome) is a functional disorder that affects the digestive system. It causes symptoms like abdominal pain, bloating, gas, and changes in bowel habits such as diarrhoea or constipation.
It doesn’t cause any visible damage to the intestines and is often triggered by stress, certain foods, or hormonal changes.
It’s a functional disorder, meaning the digestive system looks normal but doesn’t always work properly. Think of it as a moody performer, it’s not injured, just dramatic at times.
So, then what is Irritable Bowel Disease?
IBD (Inflammatory Bowel Disease) is a structural disease. It is a chronic condition characterised by ongoing inflammation of the gastrointestinal (GI) tract. It includes two main disorders: Crohn’s disease, which can affect any part of the GI tract, and ulcerative colitis, which specifically affects the colon and rectum.
Unlike IBS, IBD causes structural damage to the intestines and may lead to serious complications such as ulcers, strictures, or malnutrition.
While IBS is uncomfortable and impacts quality of life, IBD can lead to serious complications and often requires more intensive medical treatment.
Common Symptoms for Irritable Bowel Syndrome and Irritable Bowel Disease
The evil twins do have some similarities and are diagnosed primarily in young people. Other symptoms include -
-
Stomach ache
-
Bloating
-
Diarrhoea/constipation
-
Irregular bowel movements
-
Feel an urgent need to go right away, despite having done (a poopie episode)
Polar Opposites: Irritable Bowel Syndrome and Irritable Bowel Disease
The not-so-common symptoms are -
IBS
-
Nausea
-
Gassier than usual
-
Mucus in the stool
-
Abdominal swelling
IBD
-
Black/ Bloody stools
-
Weight loss
-
Loss of appetite
-
Fever
-
Inflammation in your skin
-
Risk of colon cancer

What Causes Irritable Bowel Syndrome and Irritable Bowel Disease?
IBS
There isn’t an exact cause to pinpoint, but it is often said to be caused by stress, eating habits, infections, hormones, or environmental factors (THE BASICS).
Increased gut sensitivity
People with IBS often have a more sensitive digestive tract, leading to pain or discomfort from normal digestive activity.
Disrupt harmony
Researchers believe it could be a gut and brain disturbance as well. Or how the food moves around the gut.
Food sensitivities
A gastrointestinal infection or sensitivity to certain foods like lactose, gluten, or FODMAPs (poorly absorbed by small intestines and food may ferment in the colon) can lead to the development or worsening of IBS.
IBD
Inflammatory Bowel Disease (IBD) is not fully understood, but it is believed to result from a combination of factors:
Immune system dysfunction
The body’s immune system mistakenly attacks the digestive tract, causing chronic inflammation - TALK ABOUT SELF-SABOTAGE.
Genetics
Guess what, if not generational wealth, your family can surely leave this as a gift. A family history of IBD increases the risk, suggesting a genetic predisposition.
Environmental factors
Certain environmental triggers, such as a Western diet, pollution, or antibiotic use, may contribute to the onset or worsening of IBD.
Gut microbiome imbalance
Changes in the normal gut bacteria may play a role in triggering or sustaining inflammation.
Lifestyle
Smoking (especially in Crohn’s disease), stress, and diet may influence disease development or flare-ups, although they are not direct causes.
IBD is a complex condition likely caused by the combination of these factors rather than just a single trigger.
Treatments Available
When it comes to IBS, the best treatment available and recommended often is dietary changes. Doctors may also prescribe medication, but it depends on how severe your IBS is.
Some changes you can incorporate into your life are -
-
A low FODMAP diet
-
Chuck the caffeinated drinks
-
Psychotherapy
-
Heating pad to help ease pain
-
Acupuncture
-
Chamomile tea (relax your tummy)
-
Probiotics (yoghurt)
For IBD, it is a different case. The main goal is to treat and prevent as soon as possible. And the treatment depends on the form diagnosed. But medications are the first line of treatment used. Such as -
-
Corticosteroids (taken if inflammation flares up)
-
Aminosalicylates (for mild to moderate IBD)
-
Immunomodulators (may become a long-term treatment)
-
surgery
-
dietary changes that avoid trigger foods
We advise you to take a check-up before you jump into the medications, as self-diagnosis is harmful, and the treatment isn’t one size fits all.

Diagnosis for IBS and IBD
IBS - There is no specific test for diagnosing IBS, but doctors may conclude based on family history, physical exam, and medical history.
IBD - It requires a proper medical test, such as a stool test, blood test, biopsy, X-ray, MRI Scan, and CT Scan.
Your doctor may also perform other endoscopic evaluations such as endoscopy so be prepared to empty your bowels and maybe expect some farts after you’re done (hehe).
Conclusion
I understand that it’s easy to get confused between the two; both can make you a regular visitor of the bathroom (be it anywhere), and both mess with your quality of life. But the key difference is that IBS annoys whereas IBD attacks.
If you thought IBS were a moody artist throwing a fit over coffee, IBD is the body’s version of a full-on turf war happening in your gut.
Nevertheless, both are misunderstood and deserve understanding, support, and management. Your gut is trying to tell you something, and sometimes, it’s not just a bad lunch experience; it’s a clue that something deeper is going on.
Until then, take care and STAY HYDRATED.
FAQs
Q. Can IBS turn into IBD?
A. No. IBS does not lead to IBD or cause intestinal damage. They are separate conditions.
Q. Are the symptoms the same?
A. No, although they overlap. IBS symptoms consist of abdominal pain, bloating, gas, diarrhoea, constipation, or both (but without inflammation).
IBD symptoms include abdominal pain, bloody stools, diarrhoea, weight loss, fatigue, and inflammation seen on diagnostic tests.
Q. Which one is more serious?
A. IBD is generally more serious due to its potential complications (e.g., intestinal damage, malnutrition, cancer risk). IBS, while uncomfortable and quality-of-life-impacting, does not cause physical harm to the intestines.
Q. Can diet help with both conditions?
A. Yes, but in different ways. Diet plays a major role in IBS; many patients benefit from a low-FODMAP diet.
And in the case of IBD, diet can help manage symptoms during flares, but it does not replace medical treatment.
Q. Who is more likely to get IBS or IBD?
A. IBS is more common, affecting up to 15% of the population. More frequently seen in women. Whereas, IBD is less common but is rising globally. Usually diagnosed between the ages of 15 and 35.