Understanding Varicose Veins: Symptoms and Causes
Introduction
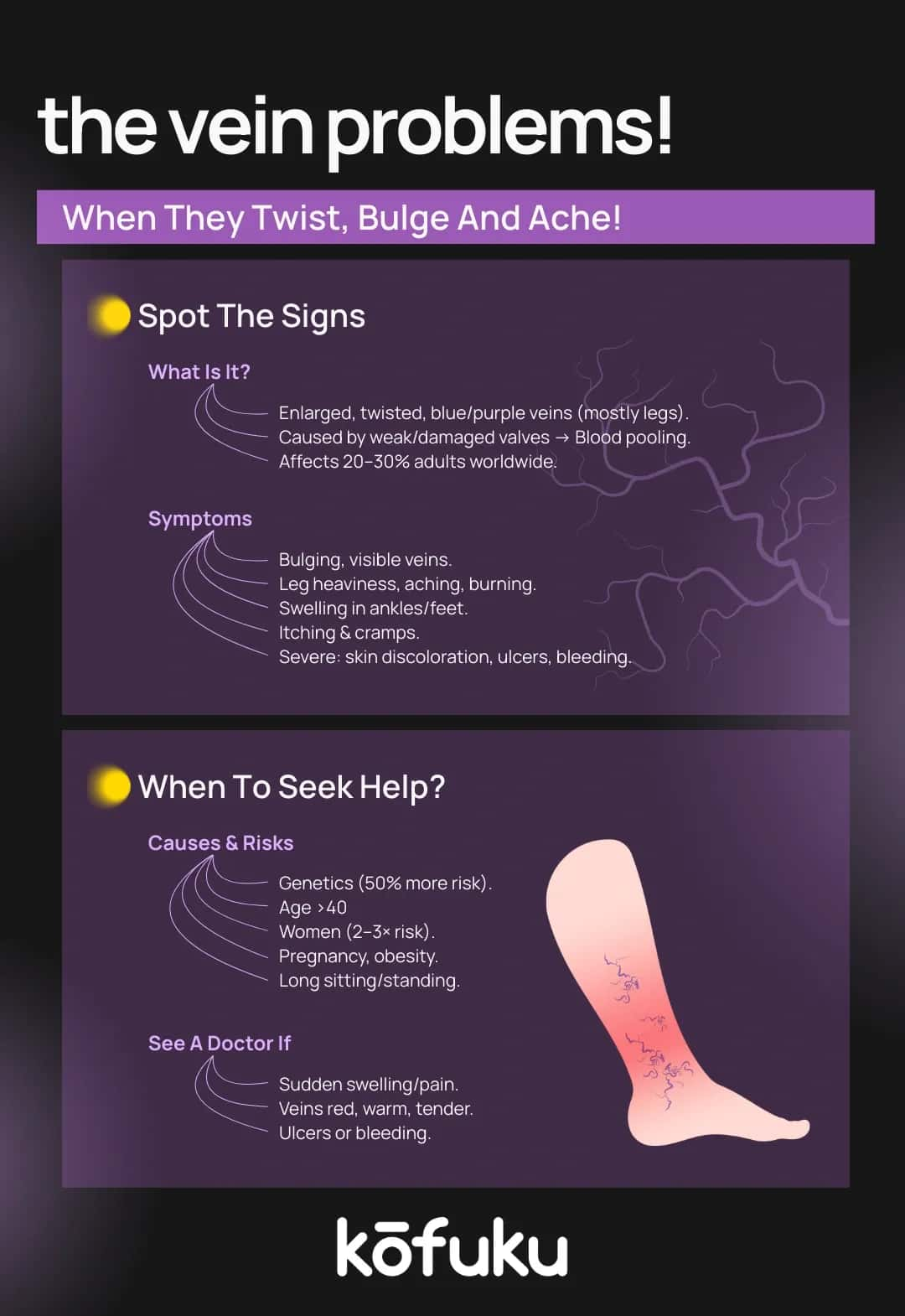
Varicose veins are enlarged twisted veins that appear on the legs when blood flow through the veins is impaired. Many people mistake them for a simple cosmetic issue, but in reality, they reflect an underlying problem with vein function.
In Indian households, leg pain or swelling is often dismissed as part of ageing, yet these visible veins can signal a medical condition that deserves attention.
Although age is a well-known risk factor, varicose veins are not limited to older adults. Prolonged standing, obesity, pregnancy, and sedentary lifestyles can contribute to their development even in younger individuals.
Varicose veins may cause discomfort, skin changes and in some cases, serious complications if left untreated. Recognising the early symptoms and seeking timely medical advice can prevent the condition from worsening.
Early Signs of Varicose Veins: What to Watch For
These are some common early signs:
- Aching or heavy sensation in the legs, especially after standing or sitting for long periods.
- Visible veins that appear slightly enlarged or bluish.
- Swelling around the ankles and feet is often more noticeable by the evening.
- Burning or throbbing sensations in the legs.
- Restless legs at night make it difficult to sleep.
At the varicose vein initial stage, veins may look like faint spider veins before becoming more prominent and twisted.
Recognising Skin Changes in Varicose Veins
In varicose veins, the skin is affected as follows:
- Discolouration or dark patches around the ankles or calves.
- Dry, itchy skin near affected veins, often resembling eczema.
- Thinning of skin, which increases vulnerability to minor injuries.
- Hardening of skin and tissues (lipodermatosclerosis), leading to stiffness and discomfort.
- In severe cases, ulcers or sores may form, usually around the ankles.
Recognising these changes is crucial because they often signal worsening venous disease. If you see discolouration or thickening around the lower legs, it may be time to consult the best varicose vein doctor in your area.

Exercise and Varicose Veins: How Movement Helps Leg Health
Exercise is one of the most potent non-invasive measures when it comes to the need to manage the health of veins. Even though some may be terrified by the thought that the condition may deteriorate due to physical activities, in contrast, it improves.
Frequent exercise stimulates and improves blood circulation and lowers venous pressure.
Best Exercises for Varicose Veins in Legs
- Walking: Simple and effective, walking daily keeps blood flowing and prevents stagnation in the leg veins.
- Cycling or stationary cycling: Strengthens the calves while being gentle on joints.
- Swimming: The buoyancy of water reduces leg pressure and enhances circulation.
- Leg raises: Lifting legs while lying down helps drain pooled blood back to the heart.
- Yoga poses: Postures like Viparita Karani (legs-up-the-wall pose) support venous return.
Is Varicose Vein Curable? Understanding Treatment Options
The most recurring question patients usually ask is: Can we cure varicose veins? The solution is that, although lifestyle modifications and medical procedures may go a long way in enhancing symptoms and looks, there is usually a long-term management process, as the disease may recur due to venous illness.
Treatment Options Include:
- Lifestyle changes: Weight management, avoiding prolonged standing, and wearing compression stockings.
- Minimally invasive treatments: Laser therapy, sclerotherapy, and radiofrequency ablation that close off affected veins.
- Surgical procedures: In severe cases, vein stripping or ligation may be necessary.
The good news is that modern medicine offers effective options, making varicose veins curable to a large extent in terms of relief and improved quality of life.

Finding the Best Varicose Vein Doctor: What to Look For
- Specialisation: Look for vascular surgeons or specialists in venous disorders.
- Experience: Doctors with experience in advanced treatments such as laser or endovenous procedures.
- Technology: Clinics offering modern imaging and treatment devices.
- Patient reviews: Positive feedback from patients who underwent successful varicose vein treatments.
Lifestyle Changes and Self-Care for Managing Early Stage Varicose Veins
- Elevating your legs when resting.
- Avoid tight clothing that restricts circulation.
- Taking short breaks to move if sitting or standing for long hours.
- Maintaining a healthy diet rich in fibre to avoid constipation, which can worsen venous pressure.
- Staying hydrated and limiting high-salt foods to prevent swelling.
When to See a Doctor for Varicose Veins
- Pain or heaviness in the legs is persistent.
- Skin changes or ulcers appear.
- Swelling worsens despite home care.
- Veins bleed or sudden pain occurs.
Early intervention by the best varicose vein doctor can prevent complications like venous ulcers or blood clots.
FAQs
Q. What are the common symptoms of varicose veins?
A. Varicose veins commonly cause bulging, twisted veins, leg pain, heaviness, swelling, throbbing, burning sensations, skin discolouration, and itching, especially after long periods of standing or sitting.
Q. What are the early signs of varicose veins in the legs?
A. Early signs include mild swelling, aching legs, visible bluish veins, itching around the ankles, and a heavy feeling in the calves, particularly noticeable in the evenings.
Q. How can exercise help with varicose veins in the legs?
A. Exercise improves circulation, strengthens calf muscles, reduces venous pressure, and helps blood flow back to the heart, easing discomfort and slowing the progression of varicose veins.
Q. What are the best exercises for varicose vein relief?
A. Walking, swimming, cycling, leg raises, and yoga poses like legs-up-the-wall are excellent exercises to improve blood circulation and relieve discomfort from varicose veins naturally.
Q. Is a varicose vein curable with treatment?
A. Yes, varicose veins can be effectively treated with lifestyle changes, compression stockings, minimally invasive procedures, or surgery. While recurrence is possible, treatment relieves symptoms and improves quality of life.
Q. What are the skin changes caused by varicose veins?
A. Skin changes include dark discolouration, dryness, itching, thinning, and hardening near affected veins. In advanced stages, ulcers or sores may develop around the ankles and lower legs.
Q. How can I prevent varicose veins from getting worse?
A. Prevention involves regular exercise, elevating legs, avoiding prolonged standing or sitting, maintaining a healthy weight, wearing compression stockings, and limiting high-salt foods to reduce swelling and pressure.
Q. Who is the best type of doctor for varicose vein treatment?
A. The best doctor for varicose vein treatment is a vascular surgeon or vein specialist, trained in diagnosing venous diseases and performing advanced procedures like laser or sclerotherapy.

Blood in Stool? 7 Tell-tale Signs of Colorectal Cancer
Understanding Your MPV Test Results: What Your Blood Report MPV Means

Blood Donation Benefits, Myths and Guidelines That You Should Know


